After my frustrations with the doctor and refusing both Aygestin (Birth Control) due to Hematologist saying no, its not an option due to it saying on the label if you've ever had clots to not take (I had a DVT/PE in 2011, and I also have FVL Heterozygous, a clotting disorder) and refusing Norethindrone (another type of progesterone only birth control I guess) and straight up telling the doctor that I refuse Lupron or any birth control, and her making me feel like I was nothing, I did several hours of research and came across Dr. Sinervo and the Center for Endometriosis Care.
Some things that patients have said about this doctor:
http://www.centerforendo.com/references.htm
So I figured, what do I have to lose, but to send them my records.
I had previously registered as a patient of theirs in November of 2014 anyway, so they had my information on file, and they were just waiting for me to send my records for review.
I took it upon myself to send a lengthy narrative, and my records from surgery in October of 2014 and my post-operative reports along with my follow-ups with the doctor and ended up sending my records today, and I hope to hear something from them soon. I will update when I hear something.
Here is a copy of my Narrative Report (So People can see an idea of what to send):
Narrative Report
Demographics
Patient: April Marie Driesse, DOB: 09/26/1989, Age: 25 years
4mos
Address: (input your address here)
Phone Numbers: (input phone numbers here)
Height: 5ft 4 inches Weight: 232lbs
Date of Narrative Report: 02/09/2015
Address: (input your address here)
Phone Numbers: (input phone numbers here)
Height: 5ft 4 inches Weight: 232lbs
Date of Narrative Report: 02/09/2015
Summary:
The patient is a 25 year old female who has been surgically
diagnosed with Stage I Endometriosis in October 2014. The surgery was done on
October 27th 2014 at Fairview Hospital in Cleveland, Ohio. The
surgery that was performed was: 1. Laparoscopy 2. Dilation&Cutterage and 3.
Hysteroscopy. Diagnosis was made via biopsy. The patient was 25 years old when
diagnosed. No hysterectomy performed. No
negative laparoscopy, as this was the patient’s first laparoscopic procedure.
No prior surgeries were ever performed to treat Endometriosis.
The patient was “diagnosed” with Endometriosis via an
Emergency Room Visit per her medical records. Prior to the surgery, the patient
had been living in excruciating pain at the time of menses. Patient described
that no medication would help, and she would often curl into fetal position and
become immobile, lying in bed for days at a time, until menses lapsed.
The patient explains that surgery was done in October 2014,
and that by February 2015, symptoms had returned. The patient was offered prior
treatment on Lupron and Aygestin but declined. Lupron’s affects were far too
risky, and patient was not comfortable taking this drug. Aygestin was
prescribed, but patient refused to take due to the bottle stating “if you have
a clotting disorder or have ever developed a blood clot, you should not take
this drug” as patient had a DVT/PE in her left leg and lung in April 2011, so
patient is not on any treatment for Endometriosis.
The patient understood that without treating the
endometriosis with birth control such as Depo Provera, or Aygestin, or Lupron
that the Endometriosis would come back and the only way to remove the
Endometriosis is via Laproscopic Procedure. The patient believes that her Endometriosis
was not excised completely, and that the Endometriosis may have grown back in
the five short months due to inability to treat and wishes to have a second
opinion.
History
The patient describes her period first started at the age of
seven, and was very heavy and painful. By the age of eleven her periods went
away all together. Farther testing being done through New Hampshire Hospital
showed that the patient’s LH levels were abnormal and follow-up by an OB/GYN
was recommended.
The patient was then diagnosed with PCOS, and placed on birth
control pills (Lo-Orval) for years to maintain her painful menses. The patient
was not definitively diagnosed with Endometriosis until her Laparoscopy in
October 2014, so the patient went from 2000 to 2014 without being diagnosed and
treated. That is fourteen years. The patient saw multiple OB/GYN’s in that
period of time, none seemed too concerned with her level of pain that she was
in and called it “normal”. There is no known family history associated with
endometriosis.
Pregnancy / Contraceptives and Relevant History
-
2000 to 2007: Lo-Orval
-
2007 to 2009: Lapse in Birth Control
o
*Patient had no insurance and became pregnant*
§
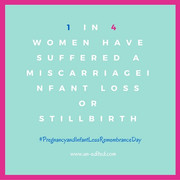
In September 2007, Patient had first miscarriage
at 5 weeks. Unknown causes.
§
In Dec 2007, patient conceived a child who was
born still on 2 May 2008 and the result of a partial placental abruption and
HLHS
§
In July 2008, patient had a miscarriage at 6
weeks. Unknown causes.
§
In Nov 2008, patient found out she was pregnant
again, and this child was due July 2009 but Born in June 2009.
·
High Risk Pregnancy
·
Followed Closely through Bedford Commons OB/GYN
and Family Health centers of SWFL/Maternal Fetal Medicine of SWFL
·
Child Delivered at 36 weeks 5 days / 34 weeks 5
days Gestational age
§
In August 2009, patient had another miscarriage
at 4 weeks. Unknown causes.
§
In September 2009, patient was placed on the
Mirena IUD
§
In April 2010, IUD Dislodged, Pregnancy
Occurred, Miscarriage at 6 weeks.
§
In June 2010, Paraguard IUD Inserted
§
April 2011, DVT/PE, Spontaneous.
§
August 2011, Paraguard IUD Dislodged, Pregnancy
Occurred, Miscarriage at 6 weeks.
§
Decided to give Mirena IUD one more try after
persuasion from an MD. (Even knowing that I had a DVT/PE in April 2011)
·
Mirena inserted in November 2011
·
Mirena IUD Removed in April 2012 for TTC
Purposes
§
Not on any form of birth control since April
2012.
Fertility Drugs / TTC
§
Clomid Started in January 2013
·
50mg – Annovulation
·
100mg – Annovulation (Feb 2013)
·
150mg – Annovulation (March 2013)
§
Femera Started in April 2013
·
2.5mg – Annovulation (April 2013)
·
5mg – Annovulation (May 2013)
·
10mg – Annovulation (June 2013)
·
12.5mg – Ovulation (Bad Egg) (July 2013)
A pregnancy occurred as the result of ovulation on 12.5mg of
Femera in August 2013. In August 2013, the patient got a positive pregnancy
test, followed by a declining beta. The pregnancy resulted in what is called a
“chemical” pregnancy. There was no more
fertility drugs issued at this point. The patient decided to give up TTC (Trying
to conceive).
The patient fell pregnant on January 7th 2014. She
ovulated on or around December 25th 2013. The patient experienced
her second chemical pregnancy on January 17th 2014 at 5 weeks 6
days.
It was determined that the patient had Factor V Leiden
Mutation and was heterozygous. It was also determined that the patient had
MTHFR A1298C Mutation. Both of these combined with hormonal and auto-immune
conditions were to blame for the patient’s lack of ovulation, as well as the
lack of sustainment of a pregnancy. The patient DOES want future children and
states she would like 1-2 more, but she has given up on trying for right now.
(6 miscarriages, 2 chemical pregnancies, 1 stillborn)
As far as holistic efforts go for the patient’s
endometriosis, the patient has tried heating pads, naturopathic medicine to
consist of acupuncture, massage therapy and chiropractics, as well as
traditional Chinese medicine. Nothing helped long term.
Diagnoses
This patient has a long list of medical diagnosis. The
following are her diagnosis and the providers who follow her.
Past
History of Deep Vein Thrombosis
Past History of Pulmonary Embolism
Female Infertility
Chronic Kidney Disease – Stage II, Controlled
Fibromyalgia
Hashimotos Thyroiditis (Auto-Immune)
Addisons Disease (Auto-Immune)
Vitamin D Deficiency
Chronic Back Pain
Primary Hypercoagulable State
Past History of Pleurisy
Post Traumatic Stress Disorder
Generalized Anxiety Disorder
Borderline Personality Disorder
Diabetes Type II
Hypothyroidism
Obesity
Polycystic Ovarian Syndrome
Chronic Migraines
GERD
Anemia
Past History of Acute Myeloid Leukemia (In Complete Molecular Remission)
Factor V Leiden Mutation, Heterozygous
MTHFR Deficiency and Homocystinuria
Myalgia and Myositis
Bilateral Carpal Tunnel Syndrome
Lumbosacral Spondylosis without Myleopathy
Cervicogenic Headaches
Sacral Illiac Joint Dysfunction
Brachial Neuritis or Radiculitis
Endometriosis – Stage I
Past History of Pulmonary Embolism
Female Infertility
Chronic Kidney Disease – Stage II, Controlled
Fibromyalgia
Hashimotos Thyroiditis (Auto-Immune)
Addisons Disease (Auto-Immune)
Vitamin D Deficiency
Chronic Back Pain
Primary Hypercoagulable State
Past History of Pleurisy
Post Traumatic Stress Disorder
Generalized Anxiety Disorder
Borderline Personality Disorder
Diabetes Type II
Hypothyroidism
Obesity
Polycystic Ovarian Syndrome
Chronic Migraines
GERD
Anemia
Past History of Acute Myeloid Leukemia (In Complete Molecular Remission)
Factor V Leiden Mutation, Heterozygous
MTHFR Deficiency and Homocystinuria
Myalgia and Myositis
Bilateral Carpal Tunnel Syndrome
Lumbosacral Spondylosis without Myleopathy
Cervicogenic Headaches
Sacral Illiac Joint Dysfunction
Brachial Neuritis or Radiculitis
Endometriosis – Stage I
Followed By:
1. Vivian
Chukwuani – PCP
2. Leila
Khan – Endocrinologist
3. David
Krahe – Orthopedics
4. Christy
Samaras – Hematology/Oncology
5. Julie
Tan – Reproductive Endocrinology Infertility
6. Viet
Nguyen – Dermatology
7. Apostolos
Kontzias – Rheumatology
8. Pasha
Saeed – Pain Management
9. Colleen
Raymond – OB/GYN
10. Natalie
Evans – Vascular Medicine
11. Tanya
Wagner – Physical Therapy
12. Kripa
Kavassari – Urology
13. Luzma
Cardona – Neurology
14. Jen
Walters – Counselor * Mental Health
15. Dr
Bernard – Medication Management * Mental Health
Pain Management
For pain management, the patient sees Dr. Pasha Saeed. The
doctor prescribes the patient the following: Tramadol 50mg, Lidocaine 5%
patches, Topamax 100mg, TENS Unit, Cyclobenzaprin 10mg, Fioricet, over the
counter medications such as Tylenol, Motrin, Ibuprofin, and the patient does
physical therapy in the water as well as nerve injections. The patient also uses
a heating pad and in the past has used controlled medications such as Percocet
and Hydromorphine. The pain regimen is not really affective, but the patient
utilizes and tolerates the pain.
Quality of Life
The patient reports trying to lose weight, to better her
life, as well as her health for the purpose of her daughter. The patient
reports that menses are still very heavy and painful, and the pain is back to a
10/10 whereas last month at the follow-up appointment the pain was gone. The
patient states “it is like the pain came back with a vengeance” The limitations
that this pain has is it affects the patients mood. The patient has been
depressed because her pain level is high. The patient reports that nothing is
working and she is frustrated with her pain level. It affects her social life
and her relationships because when she is in pain she becomes more irritable
and hard to be around.
Symptoms
The patient reports the following symptoms: Chronic pelvic
pain, Chronic low back pain, Cramping, Infertility, Painful Menses, Painful
Sex, Painful Urine and Bowel Movements, Trouble going to the bathroom (Can’t go
but have to). The only abnormalities reported by a healthcare provider recently
is that the Thyroid Meds needed to be adjusted.
Frustrations
The frustrations relating to this disease are the chronic
pain that the patient lives in. The patient also reports frustrations because
doctors do not properly treat endometriosis around where she lives. The patient
states that she is frustrated because she cannot be on birth control due to her
past history of clots. The patient wants more children in the future, but
because of her endometriosis and infertility it makes it hard to conceive. The
patient is frustrated with her body and wishes it would just work for once. She
feels that her body has rejected her and she cannot do the one thing a woman
should be able to do. She states that she feels as though when her periods come
she dreads them. She just wants her Endometriosis REMOVED ENTIRELY so she does
not live in this pain anymore.
Conclusion
The patient has tried multiple remedies. Her Endometriosis
appears to have come back within five months. The patient really wants a second
opinion from an Endometriosis Excision Specialist to see what options she has
for treatment and getting rid of her chronic pain and her endometriosis. Please
evaluate and review the patient’s medical records as well as the narrative and
the attached and help her.
Thank you in advance
 Born: June 25th 2009
Born: June 25th 2009





0 comments:
Post a Comment