As you know, in my last
blog, I vented about how stupid my OBGYN was, and is. So I decided to ask my
Endocrinologist straight up, what her thoughts were on this. I got a response back from my endocrinologist today.
I am really going to just say that I am going to switch to another hospital all together. Dartmouth Hitchcock has been nothing but bad news for either myself, or my daughter. I asked the endocrinologist up front if she thinks I have PCOS.
This is what she said. "You certainly did not present like classic PCOS. My main criteria for classifying you in this category is your high insulin level. Metformin is used for PCOS and type 2 diabetes - the main issue behind both is insulin resistance which Metformin addresses. You do not seem to have other symptoms as well as manifestations associated with the diagnosis. I think Metformin is a good addition for you. Also I definitely think getting the portion size down on your carbohydrates in meals as well as exercise is definitely going to help you. I hope this clears up some confusion. Please let me know if I can be of further assistance. Take care"
So my first question is WTF is a classic case of PCOS? I have horrible acne, skin tags, am overweight (have been my entire life) my hormones are off balance.. In doing research I found a good website that explained it all.
Classical
PCOS (Stein Leventhal Syndrome) with:
Obesity
Hirsutism
(excess hair growth), alopecia (male pattern baldness), with elevated male
hormone levels (i.e. testosterone)
Irregular
or absent menstruation since puberty
Lack of
ovulation and infertility
Ovaries
with many small cysts, hence the term polycystic
Insulin
resistance with a greater risk of developing diabetes
I see 5
out of 6 there, according to this website: http://www.seattleivf.com/pcos.html
I'm
fairly certain that I have PCOS... and that without the Metformin I would 1.
not get a period and 2. not get ovulation. I am so frustrated right now. I will
be calling my PCP at 1pm, and asking them if she can re-run labwork.
Here is my issue...
Obviously,
these doctors have not seen me over numerous years. They have not seen that my
period started at 8, and went away by 11. They don't grasp the concept that I
was put on Lo Orval at 11, until 17. They also don't get that PCOS affects
everyone differently. My periods have ALWAYS been irregular...
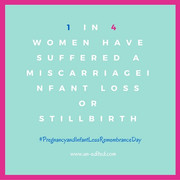
I
usually use 2007 as an example, because before 07, I don't remember when my
period was. I got my period 1 time in 2007. I ended up getting pregnant, and
miscarrying in July 07. We tried again, and In Dec 07, I got pregnant
again, but sadly delivered my stillborn in May 08.
I Had
no period from May 08 to September 08. In September, I had spotting, and don't
consider it a real period... and then in November found out I was pregnant with
my daughter Gabriella.
So from
Nov 08 to June 09, obviously being pregnant, I didn't have my period...
I got
my period in August 09... Got pregnant, and miscarried again, and after this
miscarriage, didn't want another... until I was in a steady relationship,
because I was trying to leave my at the time abusive relationship... so in
Nov 09 got my IUD inserted...
Then I
ended up having my IUD dislodge, and ended up removing it... which ended up
causing me to miscarry again... from a boyfriend who lasted only 3mos... That
was in April 2010...
I
decided to stop dating for a bit, got my life together, and again, got an IUD
placed and it caused no problems, because it was properly measured... then I
ended up meeting Alex in June 2011...
So from
April 2010 to June 2011, I did not date... Of course, after 2mos of being
with Alex, we had sex... I ended up getting pregnant yet again... and by the
time it was caught, my IUD was embedded into my uterine wall... they had to use
special tools to remove it... and they had me sign a consent form, because I
was going to miscarry... I blamed myself for that miscarriage... it was in
October 2011... Alex told me "We will
try again harder, in the future" which bothered me... but he didn't really
know how to deal with it anyway...
This
time I got a Paraguard IUD instead of the Mirena... because the IUD is the ONLY
safe birth control for those with clotting disorders so I didn't really have a choice.
Of
course, between all the pregnancies, and the IUD issues, and whatnot, I didn't
have a period... So that means my last "known" period at this point
(In Oct 2011) was in September 2008...
After
the Holidays in 2011, we decided we wanted to shoot for April 2012 for removal
of my IUD...
After a
discussion in March, we decided that I didn't want any kind of birth control to
begin with. Because of all the issues with my IUD's dislodging, and the risk of
clotting (even though they claim it was safe)
So we
had my IUD removed in April 2012. Tried for 2mos, with no success, and decided
to go to an endocrinologist. She threw me on Metformin in June... and in July
ran labwork... which came back with in normal range, but with slight
abnormalities (DHEAS was low, FSH:LH was higher than 1:1 ratio, Progesterone
was low, and Insulin was high) and so she is NOW telling me I don't have PCOS?
Yeah... that is extremely bothersome to me...
Does anyone else think that I don't fit PCOS Criteria? I posted my labwork over the last year in the documents... It just doesn't make sense to me... I'm going to see if I can find a caring doctor through Elliot, because I am DONE with being told I don't have PCOS... and I don't meet criteria... Am I wrong for being upset? Do you think that I am over reacting?
According to this website, the criteria for PCOS is as follows:
Polycystic Ovarian
Syndrome (PCOS)PCOS is a common condition affecting up to 10% of all women and
the incidence is higher in infertile women. Often symptoms present at
the time of first menstruation (menarche), but some patients develop symptoms
later in their reproductive lives and the clinical presentation varies from
subtle to overt.It is now well established that PCOS runs in families, although
different individuals may have different forms of the syndrome.
PCOS usually presents in two forms:
A. Classical PCOS (Stein
Leventhal Syndrome) with:
Obesity
Hirsutism (excess hair growth), alopecia (male pattern baldness),
with elevated male hormone levels (i.e. testosterone)
Irregular or absent menstruation since puberty
Lack of ovulation and infertility
Ovaries with many small cysts, hence the term polycystic
Insulin resistance with a greater risk of developing diabetes
Non-Classical PCOS, or
PCOS variants:
This subtle condition is
far more prevalent than the classical form of PCOS and patients present with
some of the features (1-6 above), but not all. Specifically, these patients may
be thin but still manifest the aspects of classical PCOS. Women with PCOS appear
to be at risk of developing other health problems during their lives including:
Insulin resistance and diabetes
Lipid abnormalities (cholesterol and triglycerides)
Sleep apnea
Endometrial cancer
PCOS Physiology
Patients with PCOS have
a disruption to several hormonal systems leading to abnormal ovulation,
hirsutism, and possibly insulin resistance. The associated obesity may further
compound these hormonal aberrations so that a vicious cycle is present with the
hormonal problems causing obesity, often refractive to standard weight loss
regimens, and the obesity aggravating the hormone problems. The following
hormonal problems are associated with PCOS.
- Pituitary -There is an excess production of LH compared to
FSH (greater than 3: 1) leading to disruption of the menstrual cycle and
increased androgen (male hormone) production in the ovary.
- Ovary-Increased production of estrogen without progesterone
may lead to the development of a thickened uterine lining (endometrial
hyperplasia) and possibly uterine cancer over many years. Testosterone
production is also increased in the small cysts of the ovary and this may
be converted to more estrogen in the fat cells.
- Adrenal-An elevation in adrenal androgens (DHEAS) is seen in
some PCOS patients.
- Insulin Resistance- This phenomenon relates to an insensitivity of the
PCOS patient to insulin requiring the body to produce a greater amount of
this hormone to process a given amount of carbohydrate. Since insulin has
the effect of increasing testosterone production in the ovary, a
self-perpetuating cycle is produced.
PCOS- Diagnosis
There are several
aspects important to the diagnosis of PCOS:
- History and physical
examination (this will enable classical PCOS patients to be differentiated
from the non classical)
- Hormonal testing including
fasting glucose and insulin levels
- Ultrasound to visualize
the ovaries
- Endometrial biopsy to
exclude pre cancerous uterine conditions
Treatment of PCOS
Treatment of PCOS can
take many forms including:
- Weight loss (this may be
difficult because of high testosterone levels) but may be aided by the
administration of insulin lowering medications as well as
following a low carbohydrate diet and an appropriate exercise regimen.
- Regulation of menses may be
accomplished with regular administration of progesterone or the use of an
appropriate oral contraceptive (one low in androgens).
- Ovulation induction with:
- Gonadotropins such as Follistim
or Gonal-F with the occasional use of aGnRH antagonist (Lupron) or
agonist (Ganirelix). Close monitoring to prevent hyperstimulation of the
ovary is mandatory.
- Dexamethasone may be used to suppress adrenal androgen
production.
- Insulin resistance may be
treated with weight loss and metformin (Glucophage), Actos
(pioglitazone), or Avania (rosiglitazone). These medications are
insulin-sensitizing agents that improve glucose tolerance, insulin
resistance, and lower testosterone levels. Hence, improving the hormonal
environment and often establishing normal ovulation.
- Hirsutism- May be treated with an appropriate oral
contraceptive preparation, Spironolactone, and cosmetic approaches such as
electrolysis and laser.
- Surgery- In refractory cases, laparoscopic surgery
with a YAG laser may be used to reduce the ovarian production of
testosterone by removing some of the tissue that is producing the
testosterone.
Now, I also recently was told I had mild sleep apnea that may require a CPAP or BIPAP in the future. I had my sleep study on 10-23, and the diagnosis was confirmed at today's appointment... So its frustrating to sit here and say I do not have PCOS when I know for a fact, I do.
I really really really dislike Dartmouth Hitchcock. I set up an appointment tomorrow to talk with my PCP about re-running labs, and getting her thoughts on this... I also think I am going to see if she can give me access to my medical records online, or copy the ones I don't already have for me... and mail them...
 Born: June 25th 2009
Born: June 25th 2009





0 comments:
Post a Comment